Treatment with partial prosthetics following surgery to conserve the breast
Dr. med. Vera von Bodungen, Chief Consultant at the University Women’s Hospital of LMU Munich with Susanne Ernst, Anita Medical Product Consultant
the following article was published in the 2/2016 edition of the specialist magazine MTD - Medizin-Technischer Dialog

Breast cancer in women - Treatment with partial prosthetics
Breast cancer remains the most frequent tumour condition in women worldwide.
In Germany alone, more than 75,000 women are diagnosed with breast cancer every year. The number of affected women significantly increases after the age of 35.
Latest findings confirm that most carcinoma originate in the milk ducts.
Any type of breast cancer is very much unique in terms of its aggressiveness and the speed of malignant cell growth. Overall, survival chances after surgery, drug treatments (cytostatic drugs and anti-hormonal medication, in particular) as well as radiation and new, targeted therapy options have increased significantly.
A cancer diagnosis always comes as a shock. Attending gynaecologists or plastic surgeons need to take the time to offer individualised advice to their patients, explain medical terms fully and talk about every aspect of the envisaged treatment. Breast conservation therapy can be considered in most (about 70%) early tumour diagnoses.
Usually, surgery on the breast as well as removal of the so-called sentinel lymph node from the armpit, or in individual cases, several axillary lymph nodes, is necessary. The sentinel lymph node is the lymph node to which the lymph from the area with the tumour drains first. After that, it reaches additional lymph nodes in the armpit. This lymph node therefore “keeps watch” over the other lymph nodes.
It is highly likely that this is also the first node in which tumour cells will develop. The sentinel lymph node is located, marked, removed and examined during surgery. If no cancer cells are found, other lymph nodes don’t normally have to be removed.
This procedure prevents the removal of too many healthy lymph nodes which are very important for lymphatic drainage and help to prevent lymph oedema. The lymphatic status gives an indication of how far the tumour has spread in the body. It is used for planning the next steps in the patient’s treatment.
Treatment of the affected breast includes a range of surgical options:
1. Breast conservation therapy
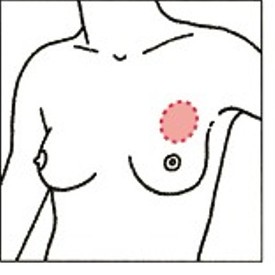
This surgical method excises the tumour with a sufficient safety margin. This option is used for minor findings or in cases of a favourable ratio of breast size to tumour size. The procedure usually leaves only minor scarring and tissue deficits. This method (also known as BCT) is followed up with radiation therapy on the remaining breast.
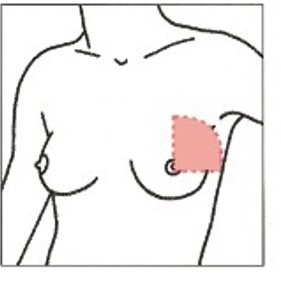
2. Quadrantectomy
The quarter of the breast where the node is located is removed. In about 55% of cases, this applies to the upper, outer quadrant. If no oncoplastic solution can be found, the relatively extensive tissue deficit will require other methods of compensation later on.
3. Subcutaneous mastectomy
The entire gland tissue is removed from under the skin. In most cases, the mastilla, skin and underlying fatty tissue can be preserved. The resulting volume deficit will require later compensation. Reconstructive surgery can be the answer in this case. There are various options for recreating a natural looking bust. An artificial implant or the body’s own tissue (e.g. from the belly area) can be used. An excised mastilla can be reconstructed at a later stage (e.g. by tattooing).
4. Ablatio simplex
In this procedure, the entire mammary gland, including the skin as well as the nipple, is removed. Based on the often significant asymmetry, prosthetic treatment is usually required at a later stage.

Primary care after surgery
A compression bra is used immediately after a reconstructive procedure for shape stabilisation and immobilisation of the breast area after surgery. It supports the healing processes using controlled compression in the area of the scar and relieves lymph drainage paths. After reconstruction with an implant, a special strap is added to ensure secure support and preventing the implant from slipping (dislocation).
After a breast reconstruction with an implant, the remaining natural breast may change over time or due to weight fluctuations, which may make a compensation for aesthetic reasons necessary at a later date. Reconstruction with the patient’s own tissue may also lead to volume deficits requiring partial compensation.
Immediately after a breast conservation surgery, soft bras made of the finest microfibre or micro modal fibre are used with or without compensatory cups with a microfibre backing as needed. These fabrics protect delicate new skin and can also be worn during radiotherapy.
During radiotherapy, the tissue is often swollen and very sensitive. A conventional bra can usually not be worn during that time. The best choice here are specialist bras with particularly soft materials that can be worn comfortably, which means the patient will not have to forego a shaping bra.
The visual result of the treatment cannot be assessed until later on in the healing process, once the tissue has recovered from radiotherapy.
The key factor: consultation
After breast surgery, the breasts often have an asymmetric appearance. Depending on the size of the tumour removed, a tissue deficit often becomes visible after surgery and once the swelling caused by it has gone down. At this point, at the latest, the patients’ consultation requirement is significant. The affected women need a contact partner who will answer their questions and will provide all the necessary information.
Balancing options and partial prosthetics
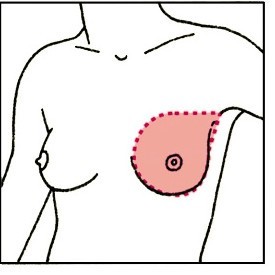
Many women decide against reconstruction but choose to compensate for the asymmetry with partial prosthetics. Soft compensation items made of silicone are very suitable. They are available in different shapes and sizes.
There is an extensive range of individual care options. The compensation shapes are made of skin-friendly, dermatologically tested silicone. They are lightweight and soft, and feature thin edges to make the transition to the skin as gentle as possible. Using these different shapes, the natural symmetry with the breast that was not operated on can be restored, uneven areas are subtly concealed and any lack of volume is gently balanced.
There are:
- Partial prosthesis in a trapezoidal shape which can be individually filled with special cotton wool, for the correction of minor deficits in the lower breast area
- Compensation prostheses in a triangular or tear-drop shape (optionally adhesive) to help balance the chest area
- Very thin, triangular cups with microfibre backing that can be padded with medical nonwoven material as needed
- Partial prosthesis with a decorative, soft microfibre backing
- Adhesive areola complex where the nipples were removed
- We highly recommend our moulded cup bras, which were developed specifically for use with partial prosthetics. The sophisticated cut does without a potentially irritating underwire or stays in the sides.

Lymph oedema
If sentinel lymph nodes are affected, a so-called axillary lymphadenectomy is required. A minimum of ten lymph nodes is usually removed from the armpit during this procedure. The removal of lymph nodes can obstruct or interrupt lymphatic drainage from the affected side. This may lead to swelling, for example of the arm. The use of a lightweight prostheses and relevant shapewear with wide, strain-relieving shoulder straps complements medical therapy.
Consequences of surgery and radiation can be lymph oedema in the breast, sides and into the back.
The following actions can help to prevent lymph oedema:
- Under no circumstances should bra straps cut in.
- Use bras with wide straps that don’t roll up, and with a soft and wide underbust band.
- Avoid clothing that could constrict on the side of the surgery.
- Do exercises that promote lymphatic drainage.
- Rest and support your arm above the level of your heart from time to time. Prevent cuts and scratches.
- Avoid carrying any weight on the side of your surgery - and that includes your handbag!
- Blood pressure measurements, injections and blood samples should not be carried out on the surgery side.
To counteract post-operative oedema development, there are also special lymphatic relief bandages for the breast and arm. A special material with a dot structure ensures better circulation, lymph is stimulated and scars can heal more effectively.